Ocular motility(movements)test:
Aim: to test the ocular motility & the actions of extra ocular muscles
Methods:
a)-Following movements(center in area 18): Binocular(test conjugate movements=versions of both eyes together) then uni-ocular(test ductions of each eye separately)
b)-Order(command)movements (center in area 8)
Steps:
a)-Following movements:
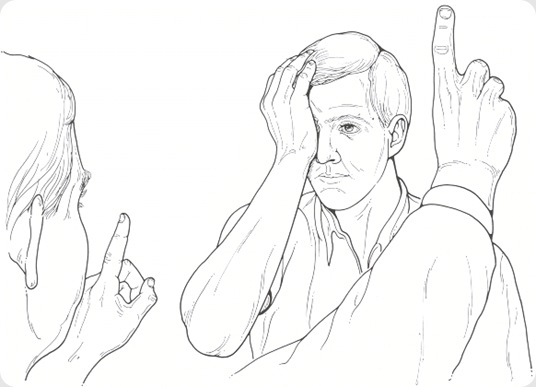
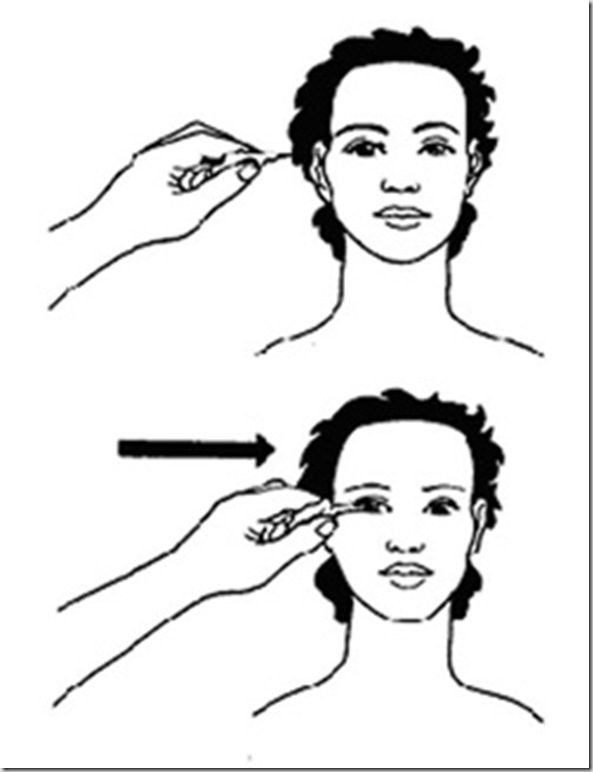
1)-Place your finger (or pen) 30-50 cm in front of the patient
2)-Ask him to follow the movements of your finger
3)-Move your finger in 6 cardinal positions:
i)-Binocular
*Start from 1ry positionàUp & right then return to 1ry position then,
*Start from 1ry positionàdirectly to the right then return to 1ry position then,
*Start from 1ry positionàdown & right then return to 1ry position then,
*Start from 1ry positionàUp & left then return to 1ry position then,
*Start from 1ry positionàdirectly to the left then return to 1ry position
*Start from 1ry positionàdown & left then return to 1ry position .
ii)-Uni-ocular
*Start from 1ry positionàUp & out then return to 1ry position then,
*Start from 1ry positionàdirectly out then return to 1ry position then,
*Start from 1ry positionàdown & out then return to 1ry position then,
*Start from 1ry positionàUp & in then return to 1ry position then,
*Start from 1ry positionàdirectly in then return to 1ry position then,
*Start from 1ry positionàdown & in then return to 1ry position .
b)-Order(command)movements:
1)-Place your finger (or pen) 30-50 cm in front of the patient
2)-Order him to move his eyes in 6 cardinal position (No movement of the examiner's hand at all)
Results:
Regarding Following movements:
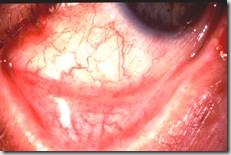
*There is normal ocular motility in all directions (bi- & uni-)
*There is limitation of ocular motility (e.g. up & out or down ) uniocularlyàmeans (paralytic squint)or binocularly(e.g. up & right)àmeans loss of conjugate movement.
Regarding order movements:
*There is normal ocular motility in all directions or
*There is loss of ocular motility up & out or down & out etc..
Oral questions:
*How to test for S.R action or I.O action or….
*Extra-ocular muscles(actions,nerve supply,cardinal position…)
*Limitation of ocular motility lost in paralytic squint intact in concomitant squint









![clip_image002[15] clip_image002[15]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEj-3qjxwNw92rSr1i1J3GfhqEDAyYOQB6DMrRtwwv_Ua6DDWyLqiWRGuTfyVIx-BFvayLfYXHWhVniTkJoI0aZNJlwESsm3TywNc-eUJJbF0jNr5DpHHaUNPj-M7w-8NtdR5zMQGl2W1lRC/?imgmax=800)